11 Ways Data Analytics Is Used In Healthcare And Why It Is Important

Healthcare doesn’t suffer from a lack of data. It suffers from a lack of useful data. Every hospital already has more data than it knows what to do with. But most of it sits unread, untapped and unused.
The result is decisions that rely more on habit than insight, overloaded systems that keep reacting instead of predicting, and patient care that follows protocol instead of the person.
That’s where healthcare data analytics either delivers or becomes just another dashboard no one opens.
Done right, data analytics helps you figure out what’s working, what’s not working, and what to do next. It shows you where resources are being wasted and where patients are at risk, as well as which treatments deliver outcomes and which ones just rack up costs.
In this article, we’ll discuss 11 practical, high-impact ways healthcare organizations are using data analytics today in care delivery, operations, research, fraud prevention, and more.
11 Ways Data Analytics is Used in Healthcare
For all the hype around healthcare data, very few people can explain what it actually does. In this section, we’ll talk about exactly that.
1. Personalized Treatment Plans
Healthcare has long relied on treatment guidelines built around population-level data. While this standardisation has benefits, it also creates a clinical blind spot, which is that most patients don’t neatly match the average.
Five patients with the same diagnosis can have completely different risk profiles, comorbidities, and likely outcomes. Yet, under traditional systems, they are often given the same baseline treatment.
Data analytics solves this by bringing individual context into the decision-making process. It pulls from actual patient histories, genomics, treatment response rates, and real-world outcomes so care plans can be matched to how patients are actually likely to respond.
Hospitals are already doing this. Some use predictive models to choose chemo drugs based on tumor sequencing and survival rates across similar patient profiles. Even drug interaction risks are flagged in real time.
Personalized treatment leads to fewer complications, faster recovery, and lower costs per patient.
2. Predictive Diagnostics and Early Risk Detection
By tracking patterns across vitals, lab results, EMRs, and past outcomes, predictive models can flag clinical deterioration hours before symptoms appear.
Take sepsis, for example. AI models can now detect early signals with over 85% accuracy, well before traditional scoring systems. The same applies to readmissions, where analytics highlight which patients are likely to return within 30 days.
3. Improving Operational Efficiency
Every hospital has inefficiencies, but most don’t know where they are or how much they cost. So, the problem is not effort but visibility.
Beds remain idle while patients wait. Diagnostic delays pile up due to uneven demand. Staff are either stretched too thin or underutilized because no one is aligning real-time resource use with actual patient flow.
Data analytics fixes this by showing exactly where friction builds. It quantifies wait times, flags scheduling imbalances, and maps process delays down to the unit level.
Some hospitals now use real-time flow data to predict discharge bottlenecks and preemptively reroute staff or capacity. That reduces the length of stay without hiring or policy changes.
4. Fraud Detection and Billing Integrity
Most healthcare organizations think of fraud as an edge-case problem that is isolated, intentional, and rare. But it’s not; it’s a structural problem.
Revenue loss happens every day through miscoded procedures, duplicate claims, outdated charge masters, and billing practices that no one’s audited in years.
Data analytics doesn’t enable fraud detection, it enables fraud prevention. It can benchmark provider activity against peer norms, flag statistically unlikely combinations of diagnosis and treatment, and surface usage patterns that suggest overbilling long before the investigation stage.
And when that’s done proactively, it strengthens reimbursement accuracy, compliance posture, and payer-provider trust.
5. Medical Imaging and Diagnostic Accuracy
The clinical model assumes that radiologists can process every scan in the order it arrives, regardless of urgency, complexity, or risk.
But in high-volume settings, that logic breaks. It leads to bottlenecks where time-sensitive findings sit behind routine reviews because the system has no prioritization layer.
AI tools are now being used to reorder scan reviews based on urgency signals. Not to diagnose, but to surface what needs human attention first. Not all chest X-rays carry the same risk, and not all delays carry the same consequence.
6. Clinical Decision Support
Most clinical decision support systems (CDSS) claim to reduce variability in care. But they actually surface protocol reminders that clinicians already know or, worse, interrupt workflows with low-value alerts that are dismissed reflexively.
The problem is that most tools are designed around static guidelines, not real-world decision-making environments. Analytics can fix that, but only if it understands context.
When systems are trained on actual care delivery data like outcomes by diagnosis, response by comorbidity, and risk by sequence of events, they stop offering general advice. They start offering insight tied to what clinicians are trying to solve at the moment.
7. Population Health Management
Most population health dashboards show you the obvious. Patients with uncontrolled diabetes (high blood sugar levels). Heart failure patients with frequent hospital visits. Patients over 65 with two or more chronic conditions.
The real value of data analytics in population health is in identifying instability before it turns into utilization, and doing it at a level of specificity that triggers meaningful intervention.
This only happens when systems analyze changes in medication adherence, early deterioration patterns, shifts in care-seeking behavior, or subtle gaps in follow-up that are predictive.
So, the goal is to intervene before risk becomes cost, and that requires models trained on how risk actually develops across a care continuum.
8. Drug Development and Clinical Trials
The majority of trial delays and failures happen because sites underperform, recruitment lags, or data quality breaks down midway through execution.
But that’s not how most sponsors do diligence. Site selection is often based on historical relationships, self-reported capacity, or geography, not actual performance data.
This is where analytics creates real value. It surfaces sites that consistently hit enrollment targets in similar trials, flags investigators with strong patient engagement metrics, and identifies operational risk indicators before launch, such as past delays, inconsistent data capture, or dropout trends.
9. Revenue Cycle Optimization
Revenue cycle analytics works by identifying where process breakdowns reliably occur, like documentation lags, inaccurate charge capture, inconsistent coding patterns across departments, or prior authorization gaps that trigger rework.
So the timing matters. The longer it takes to identify the point of failure, the more downstream cost accumulates, like denials, write-offs, resubmissions, and patient friction.
10. Resource Planning and Forecasting
The real challenge is that clinical demand is variable, and most systems are built around static assumptions.
Shift schedules don’t account for seasonal surges. Supply chain models don’t factor in procedure mix changes.
Data analytics reframes the problem by moving planning from reactive to probabilistic. It models likely patient volumes based on referral patterns, service-line growth, and local disease trends. It anticipates bottlenecks not when they happen, but weeks in advance, based on actual signals.
11. Strategic Planning and System-Level Decision-Making
Most health systems make strategic decisions using the same three inputs, historical volume, high-level demographics, and anecdotal pressure from departments.
The actual leverage point for analytics here is exposing the structural shifts that will make existing capacity, contracts, or investments obsolete, before they happen.
For example, a system may plan to expand orthopedic services based on aging demographics. But analytics may show that outpatient migration, declining referrals from key PCPs, and payer incentives are already eroding the financial viability of the service line.
These factors are what strategy needs to account for, and analytics helps replace conviction bias with directional signals.
Conclusion
Analytics only adds value when it is tied to how care is delivered, how decisions are made, and how outcomes are defined. Without that, it’s more dashboards layered on top of broken assumptions.
Every one of the 11 use cases mentioned above maps to a structural inefficiency.
The opportunity here is to rethink what should be visible, measurable, and actionable inside the system. And the organizations that do that well will be structurally advantaged.
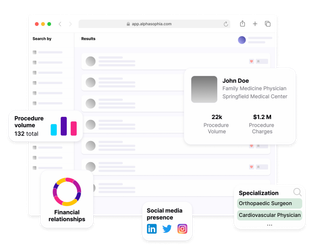
Recruit the right HCPs and HCOs with Alpha Sophia