Optimizing Clinical Trial Site Selection: How CROs Can Leverage AI-Driven HCP & HCO Data

Clinical trial site selection is one of the most critical steps in drug development but also one of the most inefficient.
If a site underperforms, recruitment slows down, timelines stretch, and costs spiral. And yet, the way most sponsors and CROs choose sites hasn’t evolved much. It’s still largely based on historical site performance, investigator relationships, and feasibility surveys that don’t always reflect real-world conditions.
The problem is that a site that recruited well in one trial might struggle in another due to protocol complexity, competing studies, or shifting patient populations. At the same time, newer, better-equipped sites often get overlooked simply because they lack a track record with a sponsor.
The result is that 80% of clinical trials fail to meet enrollment targets, and delays cost millions of dollars per day.
But the good news is AI is changing that. Instead of relying on fragmented, outdated data, AI-driven site selection not only tells you where trials have succeeded before but also predicts where they are most likely to succeed next.
Stay with us as we discuss more details on why traditional site selection is failing and how you can use AI in site selection.
Challenges in Clinical Trial Site Selection
Choosing the right sites for a clinical trial is not as simple as selecting locations with prior experience. You have to ensure that a site has the right patient population, investigator expertise, infrastructure, and regulatory readiness.
These are the things that sponsors and CROs need to predict before making a selection, but the current approach to site selection makes it difficult.
1. Patient Recruitment is Unpredictable
One of the single biggest reasons for trial delays is poor enrollment. A site that looks great on paper may still struggle to recruit eligible patients, either because the target population isn’t as readily available as expected or because competing studies are drawing from the same patient pool.
Up to 50% of clinical trial delays are due to recruitment failures, costing sponsors millions in lost time.
2. Investigator Workload is Overlooked
Sites with experienced investigators are often a go-to choice, but there’s rarely a clear view of how many studies an investigator is already running. Overloaded investigators may not have the bandwidth to support a new trial properly.
Feasibility surveys rarely capture the true operational burden on investigators, making it difficult to assess whether a site can realistically take on another trial.
3. Site Performance Data is Outdated and Fragmented
Many site selection decisions still rely on historical performance rather than real-time data. Just because a site enrolled well in the past doesn’t mean it will perform well for a different protocol or patient population.
Factors like shifting demographics, staff turnover, or changes in local healthcare systems can significantly impact site performance, but sponsors often don’t have visibility into these details.
4. Regulatory Barriers Create Delays
Every country has different regulatory requirements, and compliance can make or break a trial. Selecting a site without fully understanding its regulatory track record can lead to costly protocol deviations and extended approval timelines.
A site that has never worked with a particular regulatory authority may require even more oversight.
5. The Feasibility Process Lacks Standardization
Feasibility surveys are often self-reported, inconsistent, and subjective. Some sites may overstate their capabilities, while others may be ideal candidates but go unnoticed because they aren’t part of a sponsor’s existing network.
The lack of a standardized, data-driven feasibility framework means that the best sites for a given trial may never even be considered.
So, the underlying problem behind all these challenges is that site selection today is largely reactive. It’s based on what has worked in the past rather than what will work best for the specific trial at hand.
The Role of AI in Optimizing Site Selection
AI in site selection solves the fundamental blind spots in how sites are chosen. The industry still depends on static investigator databases, outdated feasibility surveys, and anecdotal knowledge, none of which reflect real-time patient availability, investigator capacity, or operational risks.
That’s why trials often fail at the site level.
One of the biggest shifts AI introduces is real-time adaptability. Today, site selection relies on static feasibility assessments, but AI allows you to evaluate a site continuously. If enrollment lags or protocol deviations increase, AI can flag issues early and suggest mid-trial adjustments as well.
Another overlooked advantage is how AI finds you the non-obvious site candidates. The industry repeatedly turns to familiar sites because they’ve been vetted before.
But AI scans thousands of data points to surface high-potential sites that might otherwise be ignored. So, now you have a bigger and expanded pool of viable sites.
How CROs Can Leverage AI-Driven Data for Site Selection
If you’re still relying on static feasibility surveys and past site performance to select trial sites, you’re working with incomplete information.
AI gives you real-time visibility into site conditions, patient access, and investigator workload. Instead of looking at where a trial has worked before, AI tells you where it will work now.
1. Finding Patients Where They Are
Most site feasibility assessments rely on broad epidemiological data, but disease prevalence doesn’t equal patient availability. AI maps real-time patient movement, treatment patterns, and referral flows to show exactly where eligible patients are actively seeking care.
For example, if you’re running an oncology trial. A site may have enrolled well in previous studies, but AI might reveal that competing trials are now drawing from the same patient pool, which is making recruitment much harder.
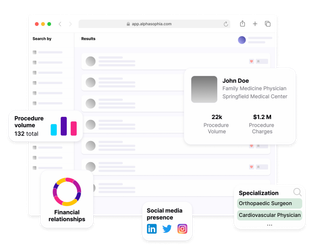
So, instead of working with outdated projections, AI gives you a live view of patient access. Tools like Alpha Sophia give you a powerful, data-driven way to identify the best sites and investigators faster and with greater accuracy.
2. Eliminating Investigator Bottlenecks Before They Happen
AI scans ongoing trial commitments, investigator workload, and staff turnover trends to highlight which sites are stretched too thin and which ones are primed for success.
So, if an investigator is juggling multiple high-demand trials, AI flags that risk before you select the site so that you can adjust your strategy instead of dealing with slow enrollment once the trial is underway.
3. Adapting in Real Time
AI not only helps you at the start, but it also tracks site performance throughout the trial and alerts you to early warning signs.
If a site is lagging in recruitment, AI can suggest activating a pre-identified backup site before delays compound. If compliance issues arise, AI highlights patterns so you can proactively intervene rather than scramble to fix problems mid-trial.
4. Ensuring Faster Regulatory Approvals
A site may have all the right infrastructure, but if it struggles with regulatory approvals or protocol adherence, your study is at risk.
AI reviews past regulatory submissions, approval timelines, and compliance records to flag sites that consistently meet approval deadlines and follow protocols so you’re not blindsided by unexpected delays.
Key Benefits of AI-Driven Site Selection for CROs
AI helps CROs avoid these pitfalls by providing real-time, predictive insights that traditional selection methods simply can’t offer.
1. Find High-Performing Sites That Are Usually Overlooked
Too many trials rely on the same investigator networks, not because those sites are always the best choice, but because they’re familiar.
That limits your options and ignores high-potential sites that have the right expertise and patient population but aren’t on your radar.
Instead of selecting a site based on historical recruitment numbers alone, AI shows you where eligible patients are actively seeking care, which sites have the right infrastructure to treat them, and whether enrollment will face unexpected competition.
2. Predict Enrollment Success
A site might have recruited well before, but that doesn’t mean it will again. Competing trials, referral shifts, and patient demographics change constantly. Traditional selection methods don’t account for this.
AI models analyze real-time patient movement, treatment patterns, and competing study activity to predict which sites are most likely to meet enrollment goals within your timeline.
Instead of discovering halfway through the trial that a site is struggling, you see the risks upfront and adjust accordingly.
3. Keep Trials on Schedule With Proactive Adjustments
If recruitment begins to lag, AI can suggest activating pre-identified backup sites instead of waiting until delays are unavoidable. If compliance trends indicate a risk, you can step in before a minor deviation turns into a major regulatory issue.
How Alpha Sophia Empowers CROs
Alpha Sophia gives you a powerful, data-driven way to identify the best sites and investigators faster and with greater accuracy.
Here’s how Alpha Sophia helps streamline and optimize the process:
1. Site and Investigator Selection
Alpha Sophia’s filtering system pinpoints HCPs and HCOs based on research contributions, patient demographics, therapeutic area expertise, affiliations, and regulatory credentials.
This means you can move beyond static investigator databases and proactively identify the best possible trial sites based on real-world performance data.
2. Smarter, Faster Recruitment and Site Activation
Alpha Sophia helps you get ahead of recruitment challenges by streamlining the process of identifying and onboarding high-quality investigators and research sites.
It helps you analyze investigator experience, trial capacity, and regulatory compliance to ensure faster site activation and a higher likelihood of hitting recruitment targets. This means less time wasted on underperforming sites and more confidence in trial execution.
3. Data Integration for Better Decision-Making
Clinical research involves massive amounts of data, but much of it is scattered across multiple sources and difficult to interpret in real time.
Alpha Sophia centralizes and analyzes these datasets, making it easier to identify the best-qualified sites based on actual performance metrics, compliance history, and operational readiness.
4. Compliance and Risk Reduction
By filtering for regulatory credentials and adherence to trial protocols, the platform helps CROs avoid compliance pitfalls and select sites that are best positioned to meet trial requirements smoothly and efficiently.
FAQs
Why is site selection critical for clinical trial success?
Site selection is crucial because it impacts patient recruitment, protocol adherence, and timelines. Poor site selection can cause delays, increased costs, and failed trials.
How can AI help CROs improve patient recruitment?
AI analyzes real-time patient data and site performance to predict where recruitment will be most successful, helping avoid underperforming sites and accelerating enrollment.
Does AI replace human decision-making in site selection?
No, AI enhances human decision-making by providing data-driven insights, allowing experts to make more informed site selection decisions.
Conclusion
When it comes to clinical trial site selection, it’s no longer enough to just rely on what worked before.
We all know the frustration of choosing a site that looked good in theory but ended up dragging the trial down due to slow recruitment, investigator overload, or regulatory delays.
AI gives you the tools to make smarter, more informed decisions. You can take real-time data, patient availability, investigator capacity, and ongoing study commitments and use it to predict which sites will actually perform under the current trial conditions.
So, AI is becoming essential for trials to run efficiently, on time, and within budget.
Accelerate AI Adoption Today