The Future of Clinical Research: AI-Powered Targeting for CROs & CDMOs

Clinical research has always been a high-stakes, high-cost game.
Every day, a new therapy is delayed, millions of dollars are lost, and, more importantly, patients who need breakthrough treatments are left waiting. CROs and CDMOs sit at the heart of this industry, managing clinical trials and drug development, and their biggest challenge is efficiency.
Delays in site selection, every misstep in patient recruitment, and every inefficiency in data management add time and expense to the process. And in an industry where bringing a single drug to market can cost upwards of $2.3 billion, inefficiency is simply unsustainable.
This is where AI is stepping in to provide real-time intelligence, precision, and scalability. But the only catch is it needs to be implemented correctly to dramatically improve efficiency, reduce costs, and enhance the quality of clinical trials.
In this article, we’ll break down the biggest bottlenecks in clinical research today, how AI-driven targeting is solving them, and what this means for the future of the industry.
Key Challenges in Clinical Research
No matter how much technology has advanced in drug discovery, when it comes to actually running clinical trials, the system still feels painfully slow.
The biggest hurdle is that they haven’t changed much over the years. Let’s take a closer look at the biggest issues that continue to slow things down.
Patient Recruitment
One of the most persistent and costly challenges in clinical research is identifying and enrolling eligible patients. It sounds pretty simple, but defining inclusion and exclusion criteria, finding participants who meet them, and enrolling them in the study is far more complicated.
Right now, most trials still rely on physician referrals, hospital databases, and ad campaigns.
It is an outdated approach that means nearly 80% of clinical trials don’t meet their enrollment targets on time, and one-third of trials fail due to insufficient enrollment.
So, naturally, sponsors and CROs are often forced to open additional sites or extend timelines, both of which significantly increase costs.
Moreover, a lot of patients drop out mid-trial due to logistical issues, side effects, or simple disengagement.
Trial Site Selection
You would think that after all these years, trial site selection will be data-driven and precise. But in reality, it’s often based on habit, familiarity, and past relationships rather than actual performance metrics.
The result is underperforming sites, regulatory or operational issues, and costly mid-trial site additions.
Many trials default to well-known academic medical centers, assuming they’ll perform well, but these sites often have competing studies and long start-up times. Meanwhile, smaller community-based sites are overlooked simply because they haven’t been used before.
Data Management
Clinical trials generate an absurd amount of data. EHRs, imaging scans, lab reports, patient-reported outcomes, and investigator notes. It’s too much information scattered across too many systems.
So, there is a clear lack of integration that makes it harder to track trends, monitor patient safety, and ensure data quality. Teams spend countless hours cleaning and reconciling data just to meet regulatory requirements when that time could be spent on analysis and decision-making.
Regulatory Compliance
Clinical research has to meet strict regulatory standards, and rightfully so. But the complexity of compliance is getting harder, not easier.
Regulatory teams spend an enormous amount of time assembling reports, cross-checking data, and making sure every box is ticked. It’s necessary work, but much of it could be automated, streamlined, or improved with the right tools.
How AI Transforms Clinical Research
AI in clinical research is not to automate everything or replace expertise. That’s the biggest misconception people have about AI in trials.
AI’s real value is in making better, faster decisions that humans wouldn’t have the bandwidth to process on their own.
This distinction matters because clinical research is a slow-moving industry, built on a system that requires endless manual intervention. So, what’s actually different now?
What is AI doing that wasn’t possible before?
1. Enhancing Patient Recruitment and Matching
For years, the industry has been talking about ‘improving patient recruitment’ as if it were merely a marketing problem.The assumption has been that patients just don’t know about trials and that if we advertise more effectively, we’ll fill enrollment gaps.
But that’s not the problem at all. The real issue is accessibility.
We’ve had patient databases, hospital networks, and EHR data for years, yet trials still struggle with recruitment.
Because even when eligible patients are identified, they aren’t always in a position to participate. They might live too far from a site. They might not meet some minor logistical criteria. They might have healthcare coverage gaps that make trial participation harder.
What AI is doing now is patient viability scoring. It’s looking at factors beyond clinical eligibility, assessing:
- How likely is a patient to enroll, given their location, socioeconomic status, and care patterns?
- What specific barriers might they face in trial participation, and can those be addressed with decentralization or mobile monitoring?
- Which trial designs are unintentionally excluding viable patients due to outdated assumptions about access.
2. Optimizing Clinical Trial Design
If a trial isn’t structured properly from the start, it will waste time, money, and patient effort. AI is making trial design smarter by simulating different scenarios before a study even begins.
It can analyze:
- Optimal sample sizes
- Inclusion/exclusion criteria
- Endpoint selection
Take patient diversity, for example. Historically, many clinical trials have struggled with the underrepresentation of minority populations, leading to treatments that don’t reflect real-world patient diversity.
AI can flag where recruitment strategies are unintentionally excluding certain groups so that you can make adjustments for the trial to be more inclusive and representative.
3. Accelerating Data Analysis and Interpretation
Right now, data analysis in many trials is painfully slow. Teams spend weeks or months cleaning, organizing, and interpreting data before they can even start making informed decisions.
AI automates the entire process, which allows:
- Faster pattern recognition
- Real-time insights
- More accurate predictions
4. Enhancing Patient Monitoring and Adherence
A lot of discussions about AI in clinical research still frame it as something that happens behind the scenes, such as optimizing processes, crunching data, and improving workflow efficiency.
But AI is also becoming a frontline tool in patient retention.
Traditional methods rely on on-site coordinators checking in with patients manually. AI-powered tools, on the other hand, can:
- Track medication adherence in real-time
- Identify patients at risk of dropout
- Provide personalized interventions
The FDA has already recognized AI’s role in improving adherence, highlighting how it can reduce trial disruptions and improve data integrity.
5. Facilitating Regulatory Compliance
Every study must meet strict documentation and audit standards, and any inconsistencies can lead to delays, rework, or outright rejection by regulatory agencies.
AI is making compliance more efficient by:
- Automating documentation
- Flagging regulatory risks early
- Improving submission accuracy
6. Predictive Modeling for Outcome Forecasting
One of AI’s most exciting contributions to clinical research is predictive modeling. Instead of waiting until the end of a trial to assess results, AI can help you forecast outcomes much earlier.
It analyzes historical trial data, patient responses, and real-time study results to:
- Predict which patient subgroups will respond best to a treatment.
- Identify early indicators of success or failure.
- Optimize trial protocols based on ongoing results rather than waiting for final data.
With this approach, you can bridge the gap between precision medicine and patient-centered care, making trials more efficient.
Business Impact of AI-Driven Targeting
The biggest cost in clinical research is uncertainty. Delays in patient enrollment, underperforming sites, and compliance failures not only slow things down, but they destroy budgets and sponsor relationships.
AI shifts CROs and CDMOs from reactive problem-solvers to proactive strategists. Instead of waiting for enrollment to lag, AI predicts which sites will struggle before recruitment even starts.
Instead of scrambling to clean data at the end, AI ensures real-time regulatory readiness. This is what sponsors are paying for, certainty, control, and fewer financial surprises.
CROs using AI are locking in bigger, longer-term contracts because sponsors trust them to deliver without costly mid-trial fixes.
FAQs
How does AI improve clinical trial site selection?
AI predicts which sites will enroll faster by analyzing real-time patient availability, investigator workload, and past performance, reducing delays and site failures.
What are the benefits of AI-driven investigator recruitment?
AI finds engaged, high-performing investigators with access to the right patients, avoiding overloaded or underperforming sites.
Can AI reduce clinical trial costs?
Yes. AI prevents recruitment delays, optimizes site selection, automates data processing, and reduces compliance risks, cutting costs at every stage.
Does AI ensure regulatory compliance in clinical trials?
AI automates audit trails, flags compliance risks early, and standardizes submissions, reducing costly delays and rework.
What data sources does AI use for HCP & HCO targeting in clinical research?
AI pulls from EHRs, trial databases, medical literature, claims data, and investigator networks to find the best-fit researchers and institutions.
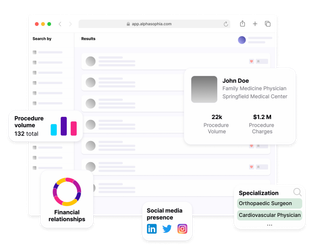
How can Alpha Sophia help CROs & CDMOs leverage AI for clinical research?
Alpha Sophia empowers CROs and CDMOs to optimize their recruitment and site selection processes with advanced filtering capabilities tailored to research, clinical, and manufacturing needs. By filtering HCPs and HCOs based on research contributions, patient demographics, therapeutic expertise, affiliations, and regulatory credentials, Alpha Sophia helps organizations identify ideal trial sites, investigators, and partners.
Conclusion
AI is no longer optional in clinical research. It’s the difference between predictable, efficient trials and delays that cost millions.
CROs and CDMOs using AI recruit smarter, select better sites, and avoid compliance setbacks, giving sponsors what they actually want, certainty.
The industry is moving fast. Those who adopt AI will lead. Those who don’t will fall behind.
Recruit suitable HCPs and HCOs for clinical trials